New York Entitlement Advocate
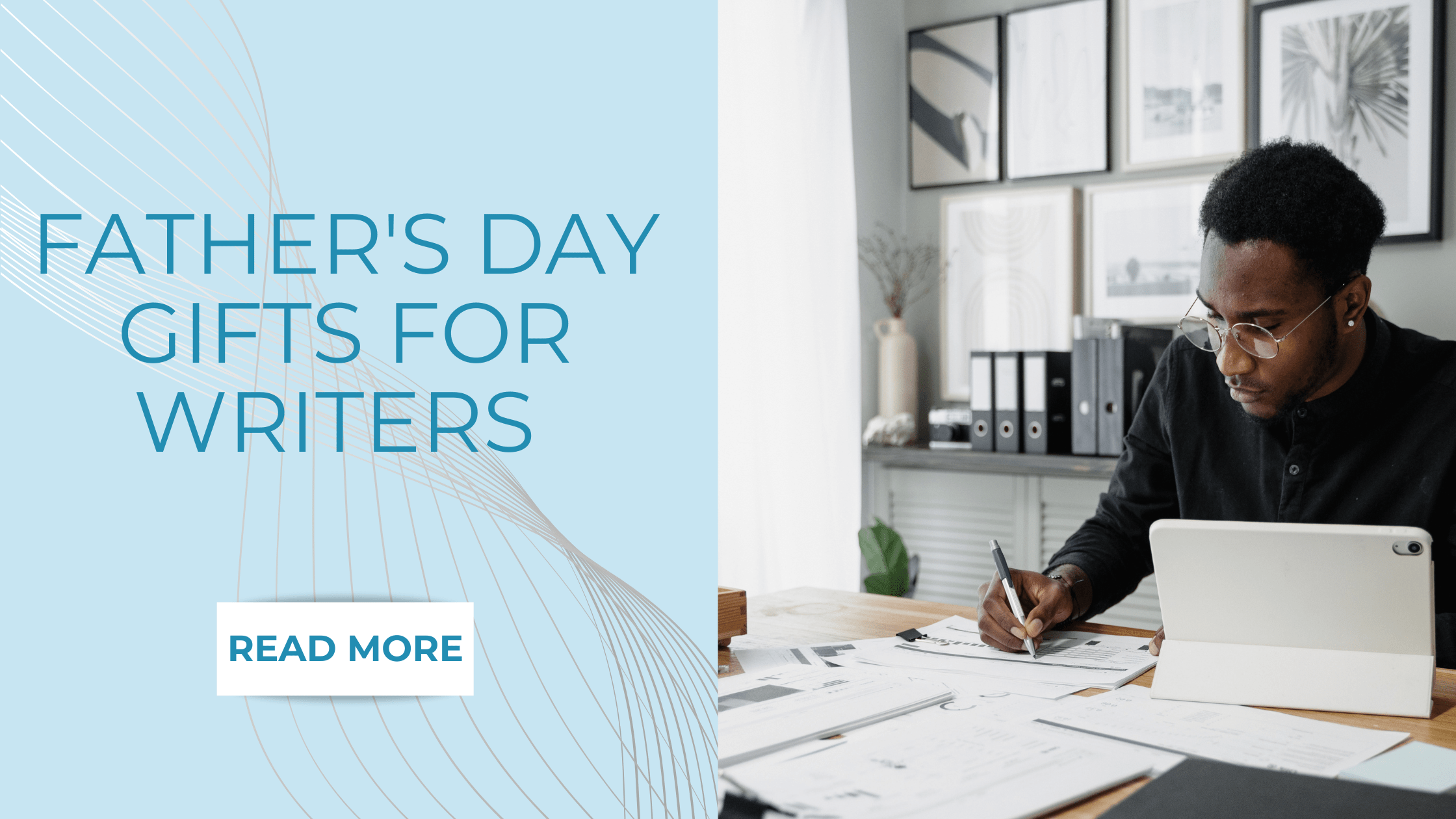
A company is looking for an Entitlement Advocate to assist members and prospects in obtaining and retaining financial entitlements. Key Responsibilities Handle inbound and outbound calls to assist customers with Medicaid and Medicare applications Educate and assess prospects for Medicaid eligibility and facilitate the completion of required documentation Monitor and assist with the renewal of members' Medicaid eligibility and maintain accurate records in database systems Required Qualifications High school diploma or GED from an accredited institution Member facing or customer service experience Ability to work a 9am-5:30pm schedule Monday-Friday and travel throughout specified regions Tech-savvy with skills in Microsoft Office Suite Bilingual candidates are preferred



































































![https //g.co/recover for help [1-866-719-1006]](https://newsquo.com/uploads/images/202506/image_430x256_684949454da3e.jpg)

























![[PATREON EXCLUSIVE] The Power of No: How to Say It, Mean It, and Lead with It](https://tpgblog.com/wp-content/uploads/2025/06/just-say-no.jpg?#)