Prioritize mental health as a business imperative
If you break your arm, you get a cast. If your cholesterol is high, you get a prescription. But what happens when what ails you is mental, behavioral, or emotional in nature? Too often, the answer is: nothing. For far too long, our healthcare system has treated the brain as somehow separate from the body. Fact is, mental health is health. One in five U.S. adults are estimated to be living with mental illness, and research suggests that 55% of adults with a mental illness have not received any treatment. The workplace is where many experienced and navigated the COVID pandemic as a collective trauma. Employees have come to expect mental health resources, and in today’s high-stress business climate alongside life’s everyday challenges, they are needed now more than ever. Left unchecked, mental and behavioral health conditions (which includes substance use disorders) cost U.S. employers approximately $282 billion each year in absenteeism, productivity declines, and associated healthcare expenses. As business leaders, we can no longer afford to treat mental health as someone else’s problem or an after-hours issue. The case for whole health Evidence (and intuition) proves the body and mind are inextricably connected. Mental health conditions like depression can double the risk of developing diabetes—and vice versa. Those living with chronic illnesses are far more likely to experience anxiety, depression, or other mental health struggles. Social determinants of health (including loneliness, housing, food security, and transportation) are additional factors. And yet, our systems continue to silo these areas of care. It’s time to bridge that divide because all of these issues impact whole health. Treating mental health alongside physical health is the right thing to do for employees—because it improves their health—and for employers, as it helps stabilize costs, reduces employee absences, and improves productivity. More importantly, it builds healthier people, at work and in life. Whether it’s expanding access with digital therapy or integrating behavioral care with primary care, the industry is finally beginning to focus more on the whole person—and not just their conditions. Invest in what (and who) matters Wellness apps and lunch-and-learns are a start, but effectively addressing mental health must go further. Serious mental illnesses (SMI), which include conditions like bipolar disorder and severe anxiety, and substance use disorder (SUD) are highly complex and require serious attention, and investment. For example, individuals with SMI face a 53% higher risk of developing cardiovascular disease—and are 85% more likely to die from it compared to those without SMI. Integrated care for these complex conditions has been shown to improve quality of life and significantly reduce overall healthcare costs. Making programs and resources available for employees with such conditions is more than good medicine—it’s good business. Nearly two million employees receive treatment for SUDs annually, and more than 13 million workers are in some form of recovery, representing 9% of all adults. This population represents a sizable portion of our nation’s workforce, and employees in recovery often show increased energy, focus, and performance. What employers can do right now As stewards of workforce health and productivity, employers have a unique opportunity to lead in this space. Here’s where to start: Enhance benefits. Modern Employee Assistance Programs (EAPs) offer far more than they once did. If you do provide an EAP, but haven’t scrutinized its options lately, you should. The latest premium models go beyond counseling, digital self-help tools, and expert referrals tailored to employees’ needs. Some now address social determinants of health and share wellbeing/mindfulness resources, concierge-level support, coaching, and on-site resources. Support all levels of need. Not every employee needs therapy, medication, or more intense care—but every employee needs support for themselves and their families. From digital wellness tools to specialized autism care access, a range of solutions helps meet people where they are. Invest in prevention. Just as we promote physical well-being through wellness incentives, the same must apply to mental and emotional health. For every dollar spent on mental health initiatives, companies can expect a return of $4 due to reduced absenteeism, lower overall healthcare costs, and increased productivity. Partners in progress: We’re in this together Ultimately, mental and behavioral health conditions are common—and treatable. By investing time, expertise, funding, and a spirit of partnership, employers can transform lives and workplaces. That’s not just good medicine—it’s good business. At Carelon Behavioral Health, we’re committed to changing how the system works. With 160 million U.S. adults spending much of their wak
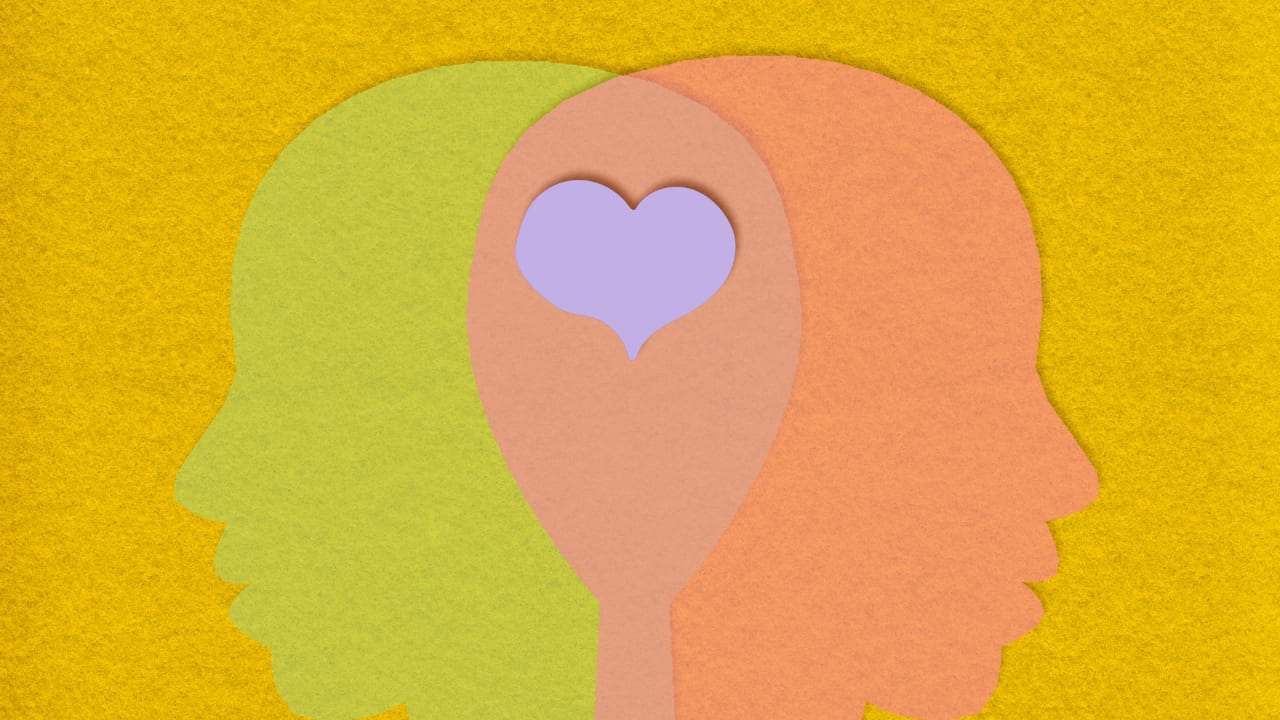
If you break your arm, you get a cast. If your cholesterol is high, you get a prescription. But what happens when what ails you is mental, behavioral, or emotional in nature? Too often, the answer is: nothing. For far too long, our healthcare system has treated the brain as somehow separate from the body. Fact is, mental health is health.
One in five U.S. adults are estimated to be living with mental illness, and research suggests that 55% of adults with a mental illness have not received any treatment.
The workplace is where many experienced and navigated the COVID pandemic as a collective trauma. Employees have come to expect mental health resources, and in today’s high-stress business climate alongside life’s everyday challenges, they are needed now more than ever. Left unchecked, mental and behavioral health conditions (which includes substance use disorders) cost U.S. employers approximately $282 billion each year in absenteeism, productivity declines, and associated healthcare expenses.
As business leaders, we can no longer afford to treat mental health as someone else’s problem or an after-hours issue.
The case for whole health
Evidence (and intuition) proves the body and mind are inextricably connected. Mental health conditions like depression can double the risk of developing diabetes—and vice versa. Those living with chronic illnesses are far more likely to experience anxiety, depression, or other mental health struggles. Social determinants of health (including loneliness, housing, food security, and transportation) are additional factors. And yet, our systems continue to silo these areas of care.
It’s time to bridge that divide because all of these issues impact whole health. Treating mental health alongside physical health is the right thing to do for employees—because it improves their health—and for employers, as it helps stabilize costs, reduces employee absences, and improves productivity. More importantly, it builds healthier people, at work and in life. Whether it’s expanding access with digital therapy or integrating behavioral care with primary care, the industry is finally beginning to focus more on the whole person—and not just their conditions.
Invest in what (and who) matters
Wellness apps and lunch-and-learns are a start, but effectively addressing mental health must go further. Serious mental illnesses (SMI), which include conditions like bipolar disorder and severe anxiety, and substance use disorder (SUD) are highly complex and require serious attention, and investment.
For example, individuals with SMI face a 53% higher risk of developing cardiovascular disease—and are 85% more likely to die from it compared to those without SMI. Integrated care for these complex conditions has been shown to improve quality of life and significantly reduce overall healthcare costs.
Making programs and resources available for employees with such conditions is more than good medicine—it’s good business. Nearly two million employees receive treatment for SUDs annually, and more than 13 million workers are in some form of recovery, representing 9% of all adults. This population represents a sizable portion of our nation’s workforce, and employees in recovery often show increased energy, focus, and performance.
What employers can do right now
As stewards of workforce health and productivity, employers have a unique opportunity to lead in this space. Here’s where to start:
- Enhance benefits. Modern Employee Assistance Programs (EAPs) offer far more than they once did. If you do provide an EAP, but haven’t scrutinized its options lately, you should. The latest premium models go beyond counseling, digital self-help tools, and expert referrals tailored to employees’ needs. Some now address social determinants of health and share wellbeing/mindfulness resources, concierge-level support, coaching, and on-site resources.
- Support all levels of need. Not every employee needs therapy, medication, or more intense care—but every employee needs support for themselves and their families. From digital wellness tools to specialized autism care access, a range of solutions helps meet people where they are.
- Invest in prevention. Just as we promote physical well-being through wellness incentives, the same must apply to mental and emotional health. For every dollar spent on mental health initiatives, companies can expect a return of $4 due to reduced absenteeism, lower overall healthcare costs, and increased productivity.
Partners in progress: We’re in this together
Ultimately, mental and behavioral health conditions are common—and treatable. By investing time, expertise, funding, and a spirit of partnership, employers can transform lives and workplaces. That’s not just good medicine—it’s good business.
At Carelon Behavioral Health, we’re committed to changing how the system works. With 160 million U.S. adults spending much of their waking hours at work, we know employers are an important key to destigmatizing mental health and unlocking whole health. It’s time we accept the fact that mental health is health. It always has been.
Bryony Winn is president of Carelon Health. Corbin Petro is president of Carelon Behavioral Health.