Endometriosis Headache: A Hidden Symptom of a Complex Condition
Endometriosis is a chronic gynecological disorder that affects millions of women worldwide. It occurs when tissue similar to the uterine lining grows outside the uterus, leading to inflammation, pain, and a wide range of symptoms. While pelvic pain and menstrual irregularities are well-known signs of this condition, many individuals also experience a less-discussed but significant symptom: the endometriosis headache.
What Is an Endometriosis Headache?
An endometriosis headache is not officially classified as a separate medical condition, but it refers to recurring or chronic headaches experienced by individuals with endometriosis. These headaches often coincide with hormonal fluctuations during the menstrual cycle and may worsen during menstruation, ovulation, or when hormone levels drop. For many women, these headaches resemble menstrual migraines, characterized by intense throbbing, light sensitivity, and nausea.
Causes of Endometriosis Headaches
Several factors can contribute to headaches in people with endometriosis:
-
Hormonal Imbalance
Estrogen plays a significant role in both migraine and endometriosis. During the menstrual cycle, estrogen levels fluctuate, and these changes can trigger migraines or tension headaches. People with endometriosis may have heightened sensitivity to these hormonal shifts, increasing the risk of headaches. -
Chronic Inflammation
Endometriosis involves chronic inflammation in the pelvic region, which can affect the central nervous system and pain pathways, potentially triggering headaches. -
Stress and Pain
Living with daily or monthly endometriosis pain can cause emotional and physical stress. Chronic pain often leads to muscle tension, poor sleep, and anxiety—all of which are known headache triggers. -
Medications
Some treatments for endometriosis, particularly hormone-based therapies, may have side effects that include headaches. For example, birth control pills or GnRH analogs can cause migraines in some individuals.
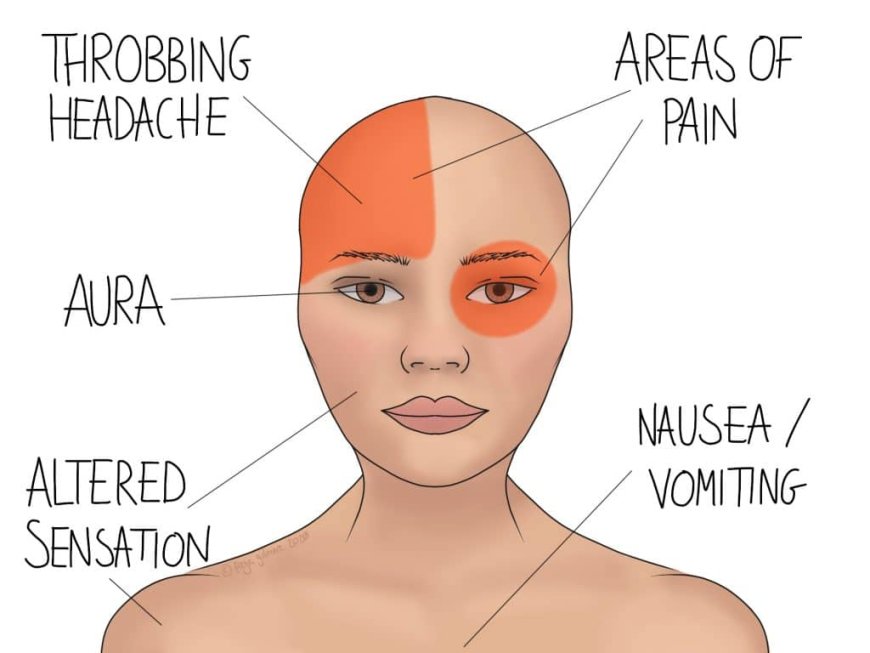
Symptoms of Endometriosis Headache
-
Persistent or cyclic headaches
-
Pain that worsens during menstruation
-
Throbbing or pulsating head pain
-
Sensitivity to light or sound
-
Nausea or vomiting
-
Neck and shoulder tension
These symptoms often overlap with menstrual migraines, making it difficult to differentiate without tracking patterns and timing.
Managing Endometriosis Headaches
-
Track Headache Patterns
Keeping a headache diary that includes menstrual cycle phases can help identify hormonal triggers and aid in diagnosis and treatment planning. -
Hormonal Regulation
Birth control pills, hormonal IUDs, or other hormone therapies may help regulate estrogen levels and reduce both endometriosis symptoms and related headaches. -
Pain Relief
Over-the-counter or prescription pain relievers, such as NSAIDs, can help manage acute headache episodes. However, regular use should be monitored to avoid rebound headaches. -
Lifestyle Modifications
Stress management, regular sleep, hydration, and a healthy diet can all contribute to reducing headache frequency and intensity. -
Professional Support
Working with a gynecologist and a neurologist can ensure a comprehensive approach to treating both endometriosis and related headaches.
Conclusion
Endometriosis headaches are a challenging and often overlooked symptom of a complex condition. By recognizing the connection between hormonal changes and head pain, individuals can take proactive steps toward relief. With proper medical care, lifestyle changes, and support, those affected by endometriosis can improve their overall quality of life and reduce the impact of recurring headaches.





























































![https //g.co/recover for help [1-866-719-1006]](https://newsquo.com/uploads/images/202506/image_430x256_684949454da3e.jpg)






















![How Smart PMs Scale Their Careers in Any Org [TPG Live Recap]](https://tpgblog.com/wp-content/uploads/2025/06/2025-06-12-thumbnail-action.png?#)