Remote RN Utilization Management
A company is looking for a Telephonic Utilization Management & Case Management Operations Registered Nurse, Remote.
Key Responsibilities
Review authorization requests using clinical judgment to ensure medical necessity and appropriate level of care
Conduct comprehensive assessments and develop case management care plans in collaboration with beneficiaries and healthcare providers
Monitor and evaluate care plans to ensure effectiveness and achieve desired outcomes
Required Qualifications
Current, unrestricted RN license with multi-state privileges or ability to obtain them
3+ years of experience as a nurse in a clinical setting
2+ years of experience performing utilization review for a health plan or inpatient facility
1+ year of experience as a case manager for a health plan or inpatient facility
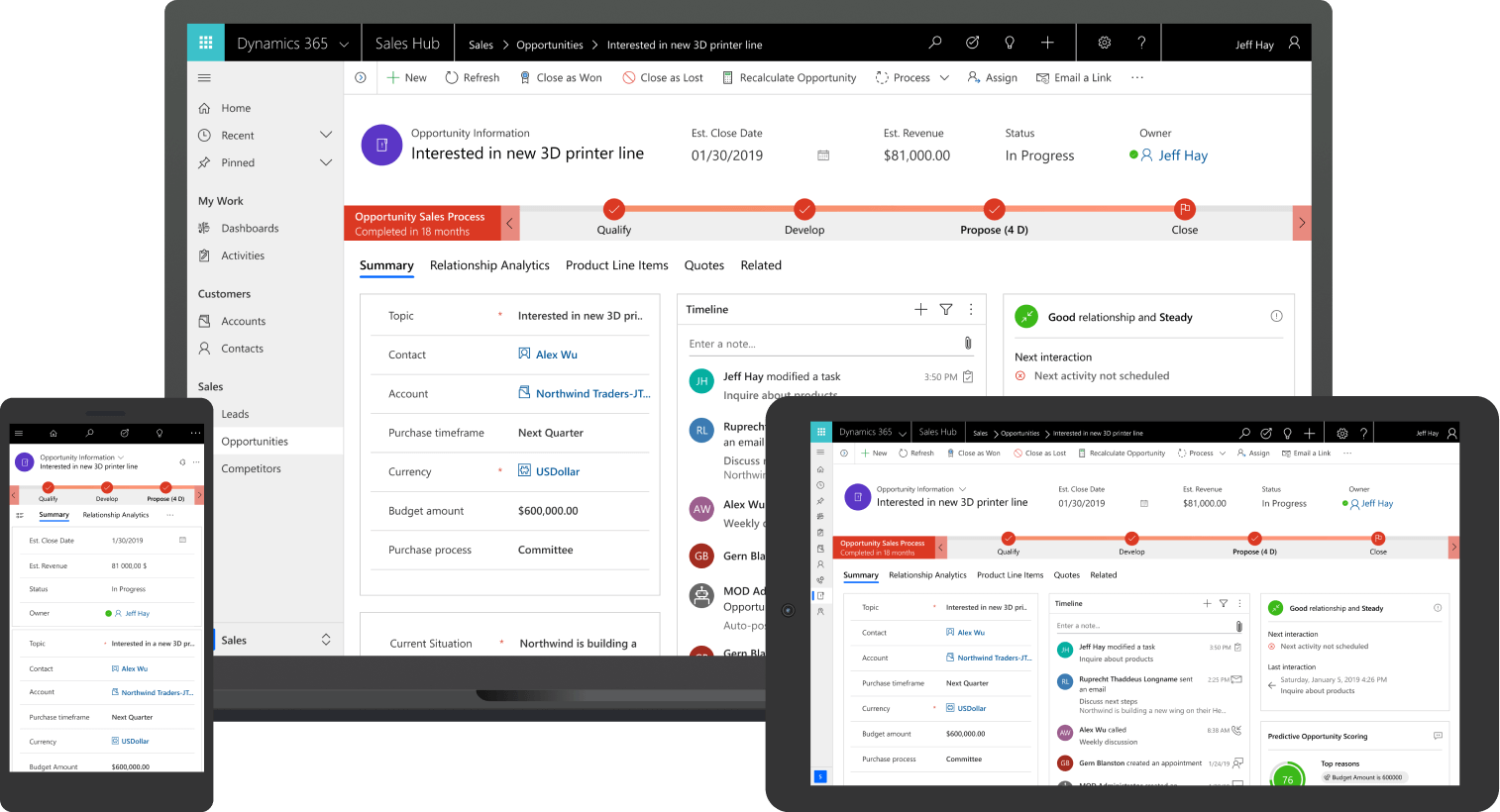
Strong technical proficiency with MS Office Suite and ability to navigate multiple systems
A company is looking for a Telephonic Utilization Management & Case Management Operations Registered Nurse, Remote.
Key Responsibilities
Review authorization requests using clinical judgment to ensure medical necessity and appropriate level of care
Conduct comprehensive assessments and develop case management care plans in collaboration with beneficiaries and healthcare providers
Monitor and evaluate care plans to ensure effectiveness and achieve desired outcomes
Required Qualifications
Current, unrestricted RN license with multi-state privileges or ability to obtain them
3+ years of experience as a nurse in a clinical setting
2+ years of experience performing utilization review for a health plan or inpatient facility
1+ year of experience as a case manager for a health plan or inpatient facility
Strong technical proficiency with MS Office Suite and ability to navigate multiple systems









































































































![Building A Digital PR Strategy: 10 Essential Steps for Beginners [With Examples]](https://buzzsumo.com/wp-content/uploads/2023/09/Building-A-Digital-PR-Strategy-10-Essential-Steps-for-Beginners-With-Examples-bblog-masthead.jpg)