This new pacemaker is smaller than a grain of rice
Researchers at Northwestern University just found a way to make a temporary pacemaker that’s controlled by light—and it’s smaller than a grain of rice. A study on the new device, published last week in the journal Nature, found that the tiny pacemaker delivered effective pacing in both animal subjects and human hearts from organ donors. The device is designed specifically for patients who need temporary pacemaking—like newborn babies with heart defects or heart surgery patients—and it’s made with materials that allow it to safely dissolve into the body once it’s no longer needed. The current standard in temporary pacemakers (called an “epicardial” pacemaker) involves sewing electrodes to the heart via wires, which then protrude out of the patient’s chest and connect to an external box. By contrast, the Northwestern researchers’ new device is small and dissolvable, and it can be implanted without any wire. The design could potentially help patients avoid complications involved with temporary pacemakers and open new possibilities for heart synchronization. From left: A traditional pacemaker and leadless pacemaker dwarf the tiny new device. [Photo: Northwestern] ‘Wires literally protrude from the body’ Generally, pacemakers are small, implanted devices that use electrical impulses to regulate the heart’s beating. Temporary pacemakers are a subcategory, and they have a few primary uses. To start, around 1% of babies worldwide are born with congenital heart defects that require surgery, after which the child needs a pacemaker for about seven days to allow the heart to self-repair. According to study lead John A. Rogers, a bioelectronics engineer, and co-lead Igor Efimov, an experimental cardiologist, pediatric use-cases were the “main motivation” behind designing the tiny new pacemaker. “There’s a crucial need for temporary pacemakers in the context of pediatric heart surgeries, and that’s a use case where size miniaturization is incredibly important,” Rogers explained in a press release. “In terms of the device load on the body—the smaller, the better.” Outside of pediatric cases, temporary pacemakers are also commonly used for a period after heart surgery in order to support recovery and minimize complications. However, Efimov notes, the standard temporary pacemakers can also present complications. “Wires literally protrude from the body, attached to a pacemaker outside the body,” Efimov said in the release. “When the pacemaker is no longer needed, a physician pulls it out. The wires can become enveloped in scar tissue. So, when the wires are pulled out, that can potentially damage the heart muscle.” A less invasive pacemaker Rogers and Efimov’s new pacemaker is designed to address the risks presented by the wires used in existing temporary pacemaker models. Instead of using wires to transmit the small electrical pulses that keep the heart on track, the new device relies on a surprising tool: light. The patient wears a small, soft device on the outside of their chest (just a bit larger than a penny), which is tasked with tracking their heart rate. When their pulse drops below a certain level, the wearable is triggered to emit a tiny pulse of infrared light through the skin and tissues to the pacemaker. Inside the body, the pacemaker has a kind of light-activated “on” and “off” switch, which is calibrated to give an electrical pulse whenever it’s in the “on” state. Alongside eliminating the need for wires, the light-based activation technology also allowed Rogers and Efimov to scale their prototype down so significantly. The researchers had previously developed a quarter-sized dissolvable pacemaker powered by a form of wireless communication, which required the device to include a receiver antenna. Once they swapped that with the infrared light scheme, it allowed them to scale the pacemaker down to just 3.5 millimeters in length, making it the smallest pacemaker ever made. The pacemaker’s size and lack of wires also allow insertion to be minimally invasive. “Typically, a surgeon will attach (sew or glue) it to the heart after surgery, when they have direct access to the heart,” Efimov explained in an email to Fast Company. In cases where a patient needs temporary pacing but isn’t having heart surgery, he added, the device is small enough that it can be inserted through just a small incision in the skin. Efimov’s team is also working on a syringe-like device that will safely inject the pacemaker into the heart for emergency pacing, like in the wake of a heart attack. After insertion, patients won’t have to worry about a potentially dangerous removal surgery, given that the tiny pacemaker is made from dissolving, bioreabsorbable materials. The current prototype is designed to dissolve after a week—which is the standard amount of time needed for the heart to return to normal pacing after surgery—but Efimov says the design might allow researchers to expand the life
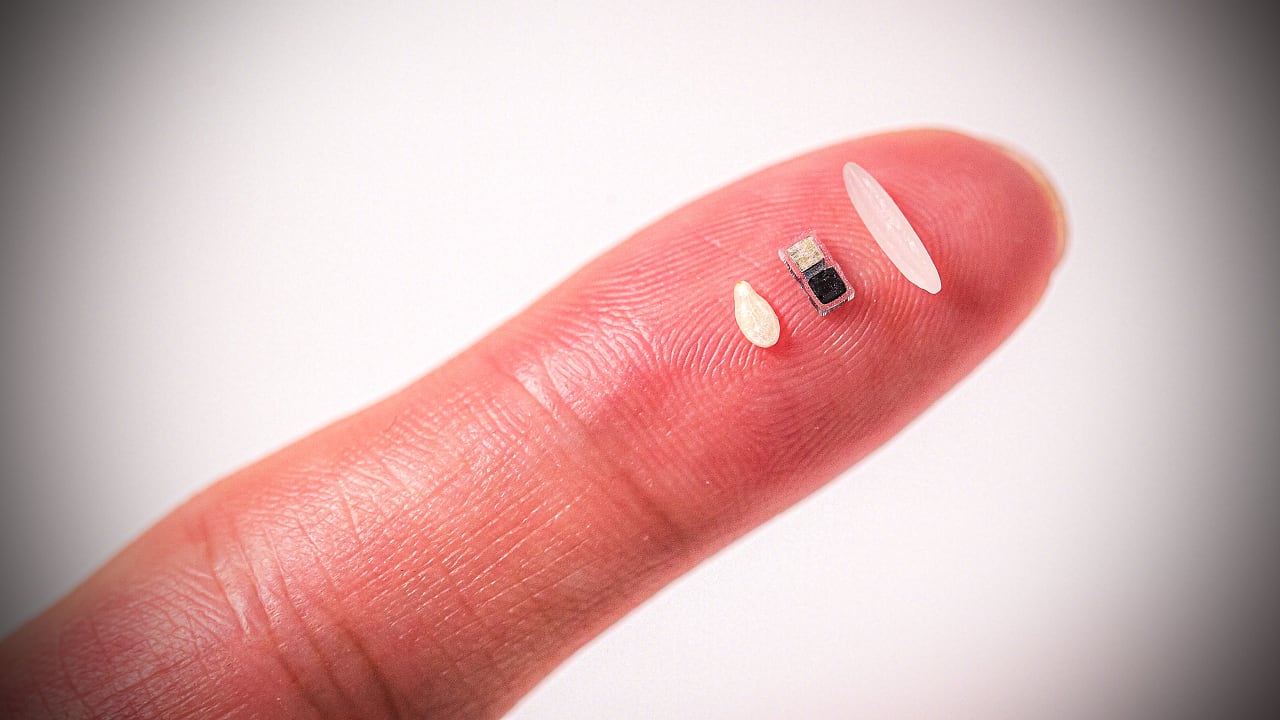
Researchers at Northwestern University just found a way to make a temporary pacemaker that’s controlled by light—and it’s smaller than a grain of rice.
A study on the new device, published last week in the journal Nature, found that the tiny pacemaker delivered effective pacing in both animal subjects and human hearts from organ donors. The device is designed specifically for patients who need temporary pacemaking—like newborn babies with heart defects or heart surgery patients—and it’s made with materials that allow it to safely dissolve into the body once it’s no longer needed.
The current standard in temporary pacemakers (called an “epicardial” pacemaker) involves sewing electrodes to the heart via wires, which then protrude out of the patient’s chest and connect to an external box. By contrast, the Northwestern researchers’ new device is small and dissolvable, and it can be implanted without any wire. The design could potentially help patients avoid complications involved with temporary pacemakers and open new possibilities for heart synchronization.

‘Wires literally protrude from the body’
Generally, pacemakers are small, implanted devices that use electrical impulses to regulate the heart’s beating. Temporary pacemakers are a subcategory, and they have a few primary uses. To start, around 1% of babies worldwide are born with congenital heart defects that require surgery, after which the child needs a pacemaker for about seven days to allow the heart to self-repair. According to study lead John A. Rogers, a bioelectronics engineer, and co-lead Igor Efimov, an experimental cardiologist, pediatric use-cases were the “main motivation” behind designing the tiny new pacemaker.
“There’s a crucial need for temporary pacemakers in the context of pediatric heart surgeries, and that’s a use case where size miniaturization is incredibly important,” Rogers explained in a press release. “In terms of the device load on the body—the smaller, the better.”
Outside of pediatric cases, temporary pacemakers are also commonly used for a period after heart surgery in order to support recovery and minimize complications. However, Efimov notes, the standard temporary pacemakers can also present complications.
“Wires literally protrude from the body, attached to a pacemaker outside the body,” Efimov said in the release. “When the pacemaker is no longer needed, a physician pulls it out. The wires can become enveloped in scar tissue. So, when the wires are pulled out, that can potentially damage the heart muscle.”
A less invasive pacemaker
Rogers and Efimov’s new pacemaker is designed to address the risks presented by the wires used in existing temporary pacemaker models. Instead of using wires to transmit the small electrical pulses that keep the heart on track, the new device relies on a surprising tool: light.
The patient wears a small, soft device on the outside of their chest (just a bit larger than a penny), which is tasked with tracking their heart rate. When their pulse drops below a certain level, the wearable is triggered to emit a tiny pulse of infrared light through the skin and tissues to the pacemaker. Inside the body, the pacemaker has a kind of light-activated “on” and “off” switch, which is calibrated to give an electrical pulse whenever it’s in the “on” state.
Alongside eliminating the need for wires, the light-based activation technology also allowed Rogers and Efimov to scale their prototype down so significantly. The researchers had previously developed a quarter-sized dissolvable pacemaker powered by a form of wireless communication, which required the device to include a receiver antenna. Once they swapped that with the infrared light scheme, it allowed them to scale the pacemaker down to just 3.5 millimeters in length, making it the smallest pacemaker ever made.
The pacemaker’s size and lack of wires also allow insertion to be minimally invasive.
“Typically, a surgeon will attach (sew or glue) it to the heart after surgery, when they have direct access to the heart,” Efimov explained in an email to Fast Company. In cases where a patient needs temporary pacing but isn’t having heart surgery, he added, the device is small enough that it can be inserted through just a small incision in the skin. Efimov’s team is also working on a syringe-like device that will safely inject the pacemaker into the heart for emergency pacing, like in the wake of a heart attack.
After insertion, patients won’t have to worry about a potentially dangerous removal surgery, given that the tiny pacemaker is made from dissolving, bioreabsorbable materials. The current prototype is designed to dissolve after a week—which is the standard amount of time needed for the heart to return to normal pacing after surgery—but Efimov says the design might allow researchers to expand the lifespan of the device up to several months.
In the future, Rogers and Efimov believe that their pacemaker design could have broad applications for various heart conditions. For those with arrhythmias, for example, multiple small pacemakers could be placed around the heart to correct its rhythm. Beyond heart conditions, the researchers posit that the light-based, dissolvable implant technology could be applied for nerve problems, wound treatment, and pain blocking.
Currently, the tiny pacemaker is still in its testing phase. Efimov says the regulatory climate makes it difficult to know when the device will be ready for use in human patients, but he believes it could be available within the next five years.
































































































![Building A Digital PR Strategy: 10 Essential Steps for Beginners [With Examples]](https://buzzsumo.com/wp-content/uploads/2023/09/Building-A-Digital-PR-Strategy-10-Essential-Steps-for-Beginners-With-Examples-bblog-masthead.jpg)





![How One Brand Solved the Marketing Attribution Puzzle [Video]](https://contentmarketinginstitute.com/wp-content/uploads/2025/03/marketing-attribution-model-600x338.png?#)
































