Director of Credentialing Operations
A company is looking for a Director of Credentialing Operations to lead provider credentialing and health plan enrollment functions.
Key Responsibilities
Oversee the end-to-end credentialing process, ensuring accuracy and compliance
Manage provider enrollment with Medicaid and commercial payers, meeting documentation requirements
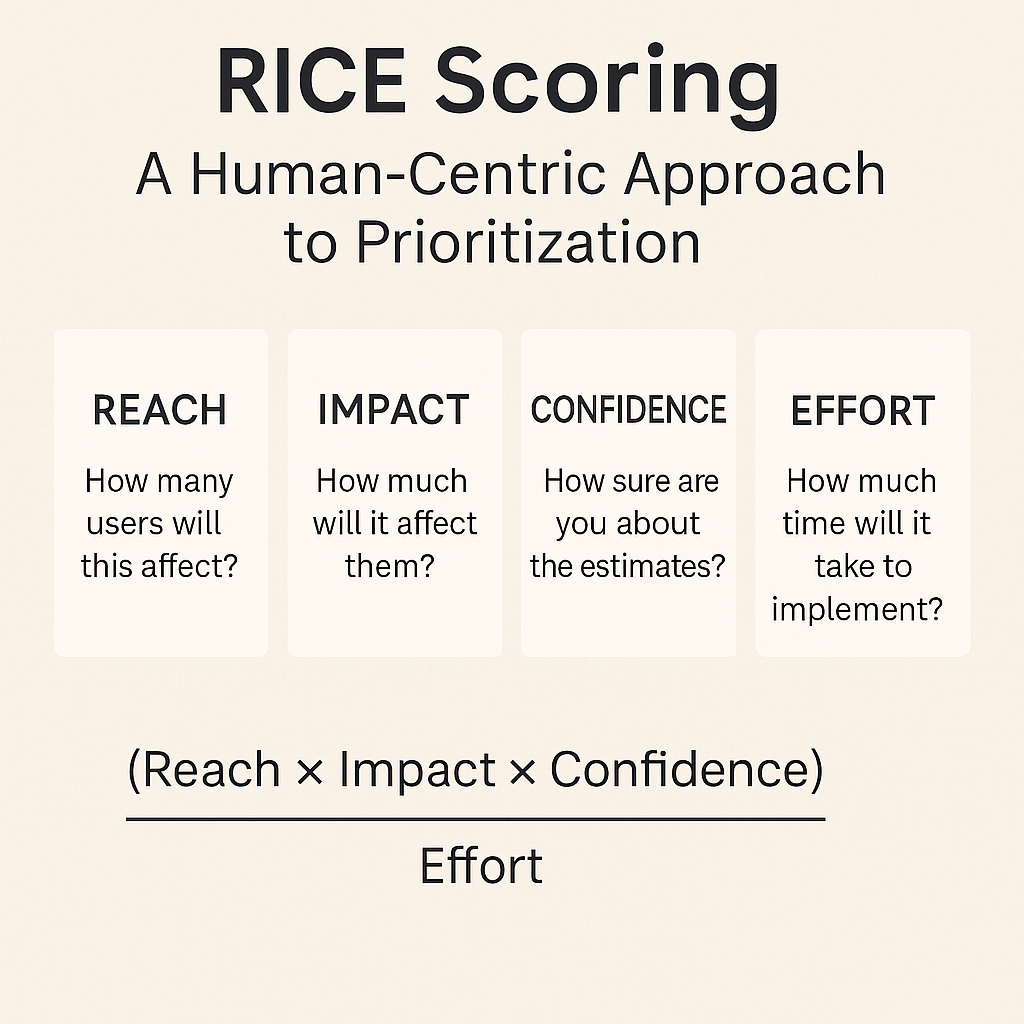
Identify and implement operational improvements and automation in credentialing workflows
Required Qualifications
5-7 years of experience in healthcare credentialing or provider enrollment
Strong knowledge of state licensing requirements, particularly Medicaid regulations
Experience managing high-volume operational processes
Proven ability to implement or improve credentialing systems and automation tools
Data-driven mindset with the ability to analyze and report on performance metrics
A company is looking for a Director of Credentialing Operations to lead provider credentialing and health plan enrollment functions.
Key Responsibilities
Oversee the end-to-end credentialing process, ensuring accuracy and compliance
Manage provider enrollment with Medicaid and commercial payers, meeting documentation requirements
Identify and implement operational improvements and automation in credentialing workflows
Required Qualifications
5-7 years of experience in healthcare credentialing or provider enrollment
Strong knowledge of state licensing requirements, particularly Medicaid regulations
Experience managing high-volume operational processes
Proven ability to implement or improve credentialing systems and automation tools
Data-driven mindset with the ability to analyze and report on performance metrics
































































![https //g.co/recover for help [1-866-719-1006]](https://newsquo.com/uploads/images/202506/image_430x256_684949454da3e.jpg)























![How Smart PMs Scale Their Careers in Any Org [TPG Live Recap]](https://tpgblog.com/wp-content/uploads/2025/06/2025-06-12-thumbnail-action.png?#)















































