Health insurance is fundamentally broken. Here’s how to fix it from the ground up
It’s no secret that when it comes to simplicity and convenience, insurance has lagged behind modern businesses across most industries. While many legacy products have been overturned by newer, intuitive solutions or adapted to meet today’s consumers’ needs, insurance offerings have remained a complex anomaly—built more for business and regulatory needs rather than real people. We already know that healthcare in America is too expensive, and far too many people simply can’t afford to get sick. Health insurance deductibles are at an all-time high, while denied and delayed claims payments persist. Insurance companies have continued making money while a staggering number of people are putting off care because of the cost, or pulling money out of their 401(k) plans early to pay for medical expenses. We also know that there is no shortage of people who are fighting for healthcare policy changes, more accountability around business practices, and broader reform. But consumer patience is running out. And with 100 million American adults in medical debt, incremental regulatory changes won’t be quick enough to take on the challenges that so many people face today in affording basic, and sometimes unexpected, costs related to their healthcare. Consumer Sentiment It’s time we ask the question: Can we start making progress by rethinking how health insurance products are fundamentally designed? In order to do this, we have to accept some consumer truths about health insurance today. First, more than 50% of Americans don’t understand their health insurance. That’s because, unlike most other industries that have embraced simplicity and ease, insurance remains complex, filled with exclusions, jargon, and unnecessary paperwork. So even with the best of educational tools, we’re looking at a large literacy gap. Second, consumer animosity toward health insurance companies is almost as old as the business itself. Even traditional supplemental health insurance offerings like Accident Insurance and Critical Illness that are intended to provide extra support were not designed to cover very much. And the amount of money that goes back to the insured at the end of the day is low for every dollar of premium paid. So it’s not surprising that people are tired of frequent claim denials and delays, and don’t trust that their coverage will minimize their out-of-pocket exposure as much as they need it to. It’s obvious that we have to start with addressing what’s covered, and how we pay claims, which is core to any insurance product. We can’t just slap technology onto insufficient coverage and hope that it’ll improve consumer confidence and trust. But there are some things we can do today to help health insurance catch up with other consumer industries through human-centered design. Here are three: 1. We can set up insurance products like subscriptions Digital simplification across industries has been happening since the dawn of Amazon and Uber, and has taught consumers to have certain expectations around their apps and online experiences. Just for the purposes of this exercise, let’s think about insurance in terms of the direct-to-consumer fulfillment model—and treat insurance like a subscription where care is the purchase and benefits are refunds. Thinking of benefits as refunds enables us to align insurance innovation with the digital simplicity today’s consumers expect. By removing the complexity wrapped around benefits, we can make claims intuitive and the delivery of benefits seamless. We have to eliminate the common limitations and restrictions as well as the excessive paperwork and evidence required for claim approval to enable quicker benefit decisions. People should be able to track the status of their claim in real time, so they can stop chasing their insurance companies for answers. Payment should be electronic, and take days, not weeks. In doing this, we can start to replicate the standards of efficiency and transparency people today are accustomed to when they buy and return products, and build a modern insurance experience that meets digital consumers’ expectations and needs. Treating health coverage like a subscription also provides clear opportunities for engagement. And insurance companies across sectors are just starting to take note. Beam Technologies tracks teeth-brushing habits through a Wi-Fi-connected toothbrush to tailor dental insurance discounts, while Discovery offers its Vitality Program that rewards customers with points for preventative checkups. By encouraging consumers to engage with their coverage, motivating them to use it by offering rewards and discounts like other consumer businesses, these companies drive utilization and deliver value as a result. 2. We can take an (active) back seat Another school of thought tells us that the best insurance companies are the ones that people don’t think about at all. Unlike the previous approach, which assumes consumers will u
It’s no secret that when it comes to simplicity and convenience, insurance has lagged behind modern businesses across most industries. While many legacy products have been overturned by newer, intuitive solutions or adapted to meet today’s consumers’ needs, insurance offerings have remained a complex anomaly—built more for business and regulatory needs rather than real people.
We already know that healthcare in America is too expensive, and far too many people simply can’t afford to get sick. Health insurance deductibles are at an all-time high, while denied and delayed claims payments persist. Insurance companies have continued making money while a staggering number of people are putting off care because of the cost, or pulling money out of their 401(k) plans early to pay for medical expenses.
We also know that there is no shortage of people who are fighting for healthcare policy changes, more accountability around business practices, and broader reform. But consumer patience is running out. And with 100 million American adults in medical debt, incremental regulatory changes won’t be quick enough to take on the challenges that so many people face today in affording basic, and sometimes unexpected, costs related to their healthcare.
Consumer Sentiment
It’s time we ask the question: Can we start making progress by rethinking how health insurance products are fundamentally designed? In order to do this, we have to accept some consumer truths about health insurance today.
First, more than 50% of Americans don’t understand their health insurance. That’s because, unlike most other industries that have embraced simplicity and ease, insurance remains complex, filled with exclusions, jargon, and unnecessary paperwork. So even with the best of educational tools, we’re looking at a large literacy gap.
Second, consumer animosity toward health insurance companies is almost as old as the business itself. Even traditional supplemental health insurance offerings like Accident Insurance and Critical Illness that are intended to provide extra support were not designed to cover very much. And the amount of money that goes back to the insured at the end of the day is low for every dollar of premium paid. So it’s not surprising that people are tired of frequent claim denials and delays, and don’t trust that their coverage will minimize their out-of-pocket exposure as much as they need it to.
It’s obvious that we have to start with addressing what’s covered, and how we pay claims, which is core to any insurance product. We can’t just slap technology onto insufficient coverage and hope that it’ll improve consumer confidence and trust. But there are some things we can do today to help health insurance catch up with other consumer industries through human-centered design. Here are three:
1. We can set up insurance products like subscriptions
Digital simplification across industries has been happening since the dawn of Amazon and Uber, and has taught consumers to have certain expectations around their apps and online experiences. Just for the purposes of this exercise, let’s think about insurance in terms of the direct-to-consumer fulfillment model—and treat insurance like a subscription where care is the purchase and benefits are refunds.
Thinking of benefits as refunds enables us to align insurance innovation with the digital simplicity today’s consumers expect. By removing the complexity wrapped around benefits, we can make claims intuitive and the delivery of benefits seamless. We have to eliminate the common limitations and restrictions as well as the excessive paperwork and evidence required for claim approval to enable quicker benefit decisions. People should be able to track the status of their claim in real time, so they can stop chasing their insurance companies for answers. Payment should be electronic, and take days, not weeks. In doing this, we can start to replicate the standards of efficiency and transparency people today are accustomed to when they buy and return products, and build a modern insurance experience that meets digital consumers’ expectations and needs.
Treating health coverage like a subscription also provides clear opportunities for engagement. And insurance companies across sectors are just starting to take note. Beam Technologies tracks teeth-brushing habits through a Wi-Fi-connected toothbrush to tailor dental insurance discounts, while Discovery offers its Vitality Program that rewards customers with points for preventative checkups. By encouraging consumers to engage with their coverage, motivating them to use it by offering rewards and discounts like other consumer businesses, these companies drive utilization and deliver value as a result.
2. We can take an (active) back seat
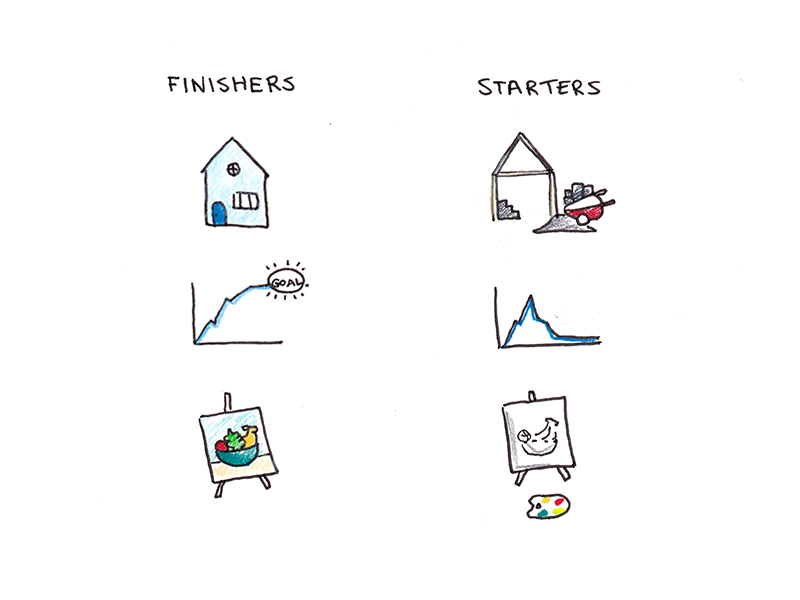
Another school of thought tells us that the best insurance companies are the ones that people don’t think about at all. Unlike the previous approach, which assumes consumers will use their coverage like they do their subscriptions, this strategy doesn’t expect that the modern consumer wants to interact with their insurance company at all. Instead, it offers a simple promise of value without any participation required.
This approach provides obvious opportunities for leveraging data and automation to set up a product experience where the claim end-to-end is managed by the health insurance company, with no necessary intervention from the insured at all.
Innovators in the space are just getting started automating several, if not all, aspects of the claims process. Current players like ClaimsMinder, Human API, and Claritev are just beginning to unlock the power of data to streamline the notification, filing, processing, and payment of a claim so that employees can get more out of their benefits. Ansel Health offers “medical claims integration,” which enables them to determine when individuals have a covered condition and are eligible for a benefit, and pays them directly without requiring them to ever file a claim.
In doing this, we eliminate coverage disputes, delayed claims payments, or even just make someone’s day a little bit easier—and maybe then begin to build some trust.
3. We can become a logical extension of the modern care-delivery revolution
When people get sick, they don’t see their preventative care or treatment and their health insurance as two separate entities, but rather one experience.
Unlike insurance, modern care delivery has evolved at a rapid pace over the past 25 years. Digital and in-person clinics like Wally, Maven, Tia, Omada, Parsley, and One Medical are setting new standards for the way people experience care, and even legacy care providers are mimicking their practices with apps and more. Notably, most of these providers have chosen to offer subscription-based or up-front payment models and to “cut out the insurance middleman.” Why? Because it just doesn’t align with their promise of simplicity and empathy through the provider experience.
By applying human-centered design, we can bridge this gap—creating insurance brands that look and feel like a natural extension of the modern care delivery experience. Companies like Oscar, Rightway, and Sana are already proving this is possible, offering an integrated experience that resonates with today’s consumers.
It’s a fair question to ask, but why will business stakeholders care?
A part of it will be about finding a set of believers and innovators who are both mission-aligned and consumer-focused. But it’s also important to acknowledge that fixing the flaws in the health insurance experience doesn’t just address the financial crisis around healthcare, it aligns with business needs too.
In fact, there’s a clear business case for creating simpler health insurance products.
According to the Integrated Benefits Institute, serious illnesses, when not treated, result in an average of 1.5 billion lost work days per year, costing employers $575 billion annually. When employees don’t delay or skip care because they’re confident in their health coverage, they’re less likely to require sick time, workers’ compensation, disability, or family and medical leave. Employers see higher retention, insurance brokers and agencies build deeper trust with their clients, and insurance companies see a higher rate of renewals. Established companies can participate too through partnerships with modern solutions, allowing them to stay competitive in an evolving marketplace, benefiting new, innovative players seeking broader distribution.
Our goal is simple: In 10 years’ time, we want people to be talking about how complex health insurance used to be, and finally build some real trust.







































































































![Building A Digital PR Strategy: 10 Essential Steps for Beginners [With Examples]](https://buzzsumo.com/wp-content/uploads/2023/09/Building-A-Digital-PR-Strategy-10-Essential-Steps-for-Beginners-With-Examples-bblog-masthead.jpg)















![How to Use GA4 to Track Social Media Traffic: 6 Questions, Answers and Insights [VIDEO]](https://www.orbitmedia.com/wp-content/uploads/2023/06/ab-testing.png)